This was an interesting case that initially caused us some confusion. The pre-op PA gave the appearance of a molar with fused roots. There was a deep pocket on the mesiopalatal aspect. The shape of the roots and the deep pocket was concerning. There was no obvious sign of a fracture progressing from the crown apically in this area. Once we accessed the tooth, we were unable to get a reproducable reading with the apex locator, despite optimal conditions.

The lack of a decent apex locator reading and the pocketing was enough for us to warrant investigation with a cone beam CT and once again, we were presented with a situation where the CBCT reveals much more useful information than the PA radiograph.


The initial dressing with calcium hydroxide has failed to resolve the pocketing so we discussed further options. The tooth was dressed again and the pocket again failed to resolve. The tooth remained uncomfortable to function.

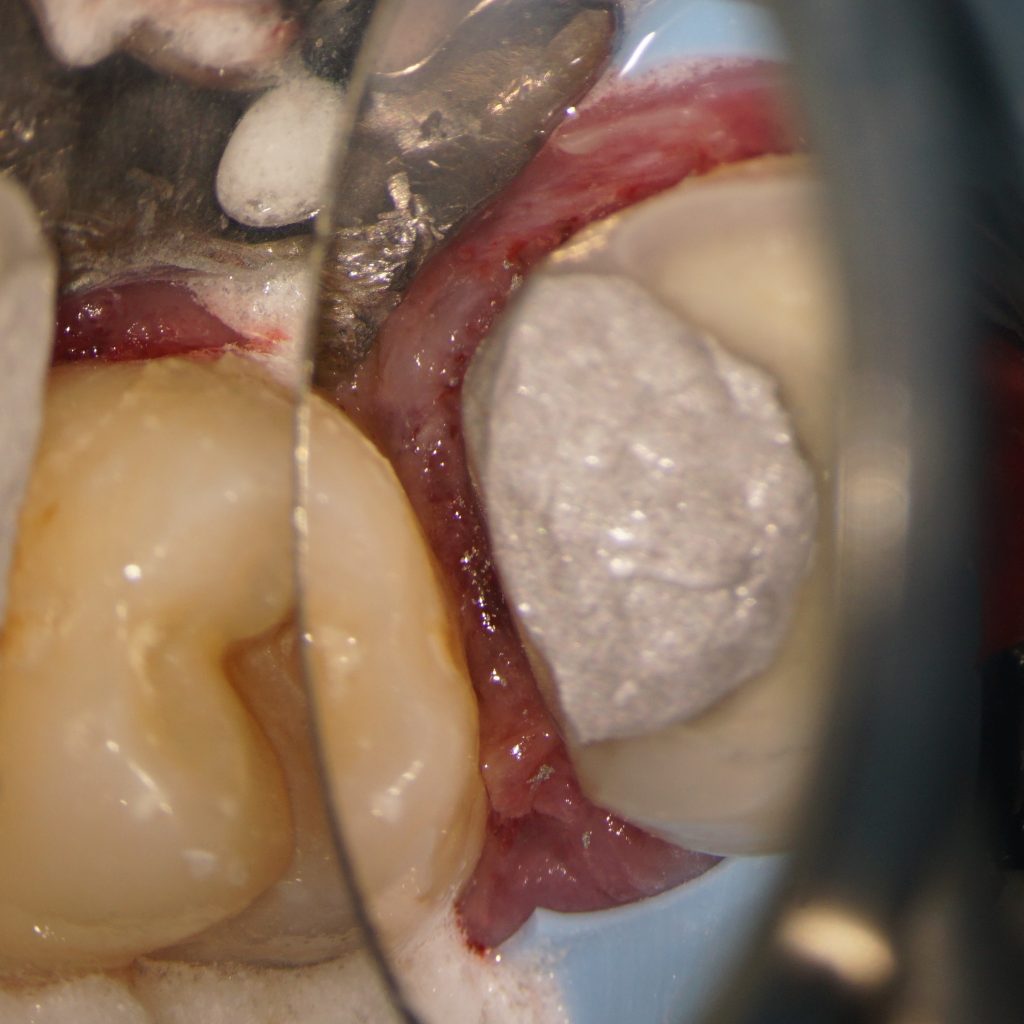
A decision was made to resect the palatal root in order to attempt to save the bridge. The patient has a good understanding that the reduced support may lead to fracture long term, but was keen to go ahead with the treatment. The palatal canal was filled with GIC and the palatal root resected. At six month review, the tooth is now comfortable and the pocket has resolved. We continue to monitor this case.