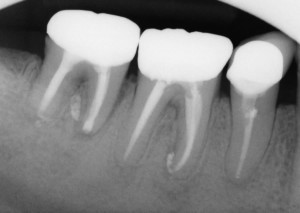
Despite Endodontic Re-Treatment The Second Molar Was Associated with a Sinus Tract. Resorption of the Distal Root Apex Can be Seen.
Intentional Reimplantation involves carefully extracting a tooth, performing root end resection and retro fill, and reimplanting the tooth. It is a simple and reliable procedure which can be performed by any dentist and can be used to retain teeth that might otherwise be deemed hopeless. See the Endospot Study Guide to Intentional Reimplantation at the end of this post for references and a full list of indications/contraindications etc.
In situations where endodontic procedures have failed or cannot be undertaken, endodontic surgery is a commonly used treatment modality. There are, however, situations where traditional endodontic surgery is difficult, or inappropriate. In particular, this occurs where anatomy such as a thick bony plate limits access (especially in the lower 2nd/3rd pre-molar), or vital structures such as neurovascular bundles are at risk (especially the mental n. in the region of the lower 1st/2nd molar). This also occurs due to other factors such as accessibility, lack of patient cooperation or a preference not to undertake surgical procedures.
In these cases, intentional reimplantation (IR) may provide an option to treat persistent apical disease. In certain cases, IR is the preferred option over surgery. IR is not a last hope procedure. When done according to protocol it is very predictable. The procedure itself is something that many dentists may find confronting, but in reality it is not difficult to do, and most dentists can have it in their repertoire.
I’ve mentioned that IR is not a last hope procedure, but in any event, when you have run out of options, and a tooth is to be extracted, then it may be worth considering treating and replanting the tooth.
The two main contraindications to IR are flared or curved roots and periodontal involvement. The first is an obvious contraindication, because the tooth needs to be able to be extracted in a controlled manner. One key factor for success is to limit the damage to the cementum layer of the toot. If the cementum layer or PDL is damaged, then there is a greater potential for resorption to occur. The second is obvious as well, because an unhealthy periodontium will complicate the healing process. Once again, see the study for a full list.
When I discuss this procedure with dentists, they are often concerned about the potential for resorptive processes and ankylosis. Most of this concern comes from experience with teeth that have been avulsed. IR is a completely different situation to a traumatic avulsion. You could reasonably expect far more trauma to the cementum and bone during a traumatic avulsion, but probably more importantly is that the tooth is often left , contaminated, dry and out of the socket for an extended period. This leads to necrosis of the PDL, and ankylosis ensues. With IR, the tooth is very carefully extracted and maintained out of the mouth in a moist environment for a very limited time. These conditions are ideal to allow healing.
A classic case is the lower second molar which has been treated endodontically and shows signs of persistent disease. In the case below, the patient was referred for management of persistent disease in the first molar. The lower right second molar has been re-treated by and endodontist 3 months prior to the patient being referred to me. Unfortunately, there was a sinus tract present, associated with the distal root of the 2nd molar (determined by taking a radiograph with a #30 GP point in the tract).

#30 GP Point Inserted into The Sinus Tract Traces to the Distal Root
I spoke to the treating endodontist who told me that the distal root had an open apex, and he had filled the distal canal with MTA. In this case, access and a large amount of bone overlying the root of the 2nd molar make surgery untenable. Even many experienced endodontists will tell you they have never performed traditional apical surgery on a lower second molar. After discussion with the patient, we decided to perform a reimplantation.
The tooth was periodontally sound, and exhibited normal mobility. It was not tender to percussion or palpation. Radiographic examination revealed a lucency associated with both roots, lucency in the furcation region and extruded material associated with both roots. Prior to extraction, the tooth is taken out of occlusion. When the tooth is repositioned, swelling may result in the tooth slightly extruding from the socket, so it is important to ensure there is good clearance from opposing teeth. Pre- & post-operative broad spectrum antibiotics such as amoxycillin are given. Chlorhexidine mouthrinse three times daily is initiated one day prior to the procedure and continued for one week after.
LA is given and the tooth carefully extracted. By this I mean that very gentle force is utilised. The tooth is grasped with forceps only by the crown. The root surface is not touched, so as to avoid damaging the cementum layer. It is common to spend 15 or 20 minutes extracting a tooth that might otherwise be extracted very rapidly. Obviously, the use of luxators and elevators is avoided.
Once extracted, I place a rubber band around the handles of the forceps to prevent the tooth being dropped. It’s important to keep the PDL moist, so have plenty of solution available and keep your assistant active in syringing solution over the PDL. A physiological solution is used. There is evidence that solutions such as hartman’s solution provide better stability of the PDL cells, but saline can also be used (a solution used in the transport of organs for transplant has been shown to by the best at maintaining viability of PDL cells, but this may be impractical).
The apicectomy is then performed using a high speed bur with copious water coolant. I know that water is not the best thing to be applying to PDL, but I think it’s more important to have coolant that to allow uncontrolled heat to be applied to the root. In general aim to remove 3mm of root tip. This should remove most of the accessory canals that may be harbouring microorganisms.
The next step is to use a small round bur to complete the retropreparation. There is no trick to this. Simply create a preparation in the root canal space 3-4mm deep. Any isthmus which is present between canals should also be prepared. This will especially occur in the mesial root of the lower molar. This preparation is designed to remove any infected GP and dentine and allow a retrofill to be placed which will seal in any remaining microorganisms or their products. Inspect the root surface for lateral canals and fill these in the same manner. In this case, the distal canal had been filled with MTA. MTA seals extremely well (compared to GP, which does allow micororganisms to pass) so there was no need to place a retrofill in the distal root.

The retropreparation has been completed in the mesial root. The distal root is filled with MTA so no retrofill is required.
There are many suitable materials for retro filling. The two most popular with endodontists are MTA and Super EBA. These materials have shown a good ability to seal and MTA in particular is highly biocompatible. MTA can be diifcult to handle, so make sure you have practised mixing and handling it first if you plan to use this. If these materials are not available, then IRM may be used. In the past amalgam has been used for retrofilling, but this material tends to corode over time, leading to loss of seal. When placing the retro fill, pack the material into the cavity with a small amalgam plugger, and then burnish.
The next step is to carefully debride the pathological tissue from the tooth socket. Here, it is important to try to avoid disturbing the PDL. By debriding, you are also removing the blood clot which may have formed in the socket. Irrigate the socket thoroughly and reposition the tooth with gentle pressure. It helps to have the patient bite gently on a wooden spatula to help ensure the tooth is correctly positioned into the socket.
Generally, no splinting will be required and a suture is placed over the tooth to hold it in position. Splinting is not desired as it impedes cleaning the area, and may lead to higher rates of resorption. If the tooth is excessively mobile after replantation, then consider splinting for a short period (3-4 days). Again, I’m aware that guidelines for traumatically avulsed teeth advise splinting, but a replanted lower molar has much greater primary stability than a replanted central or lateral incisor which was knocked from the mouth, and years of experience by endodontists conducting this procedure show that splinting is rarely required.
A radiograph is taken immediately after replantation to help confirm that the tooth is repositioned and as a baseline for healing. The sutures can be removed after 3 days and occlusion checked again. At this point some physiological movement due to occlusion is fine, but make sure the tooth is not high in occlusion. Most patients report very little discomfort after the procedure. Oral hygiene is important and flossing and brushing should resume as soon as the patient is comfortable.
The post-operative radiograph revealed I had failed to remove the extruded sealer which was associated with the mesial root. This was probably a result of careful debridement of the socket. The decision was made to leave this in place as re-extracting the tooth was likely to case more damage than benefit.
Review of the case mentioned above at 2 weeks revealed the tooth to be quite mobile. This is not unusual, as is not a cause for concern as the tooth will generally become less mobile. Importantly, periodontal examination was within normal limits. indicating that reattachment of the PDL had been successful. The sinus tract had healed. Examination at three months revealed no sinus tract, nil tenderness to percussion nor palpation, normal periodontal examination and normal mobility. Radiographic examination revealed excellent healing of the periapical areas. There continued to be lucency in the furcation area. This tooth will be monitored and I’ll update the post accordingly.
Pre-op and 3 Month Review Radiographs. Excellent, But Incomplete Healing of the PA Lesions are Apparent. Prognosis is Excellent. The First Molar Has Been Re-treated and Initial Healing of The PA Lesions is Also Apparent.

Six month review shows osseous healing adjacent to the root ends of the second molar. The tooth is functional, periodontally sound and mobility is normal. Coronal restoration should now proceed. The lesion on the mesial root of the first molar has also continued to heal but a lucency remains around the extruded sealer.
Update on this patient:
A three year review has now been undertaken. The tooth is asymptomatic, periodontal probing and mobility is normal. At this stage there appears to be no sign of ankylosis. The PA shows excellent resolution of the apical lucencies.

Occlusal view of restored first and second molar.

Side view. The tooth is healthy with no sign of return of the sinus tract and in function.
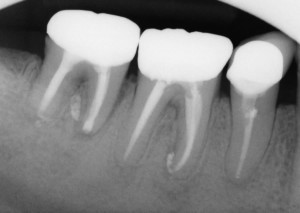
The three year review PA shows good healing of the apical lucency. The lucency associated with the mesial root of the first molar has also resolved. This simple and inexpensive treatment has allowed this patient to keep their tooth in function in the short term. I will keep recalling the patient.
Lets Hear Your Thoughts:
I’d like to hear from others on your technique and experiences with IR. Feel free to send through cases and I’ll add them to this post.
References
Bender IB, Rossman LE (1993). Intentional replantation of endodontically treated teeth. Oral Surgery, Oral Medicine, Oral Pathology 76(5):623-630
Peer M (2004) Intentional replantation – A last resort treatment or a conventional treatment procedure? Nine case reports. Dental Traumatology 20:48-55
The EndoSpot Study Guide on Intentional Reimplantation:
The best known reference for IR is Bender IB, Rossman LE (1993). Intentional replantation of endodontically treated teeth. Oral Surgery, Oral Medicine, Oral Pathology 76(5):623-630. In a retrospective case series they followed 31 cases for 1 day to 22 years and reported an overall success rate of 80%.
Another good overview is provided by Peer, however this is a simple case series. Criteria for success/failure is not listed and no rates of success are given: Peer M (2004) Intentional replantation – A last resort treatment or a conventional treatment procedure? Nine case reports. Dental Traumatology 20:48-55
Primary Indications for IR are listed as:
- Teeth have been treated unsuccessfully by conventional means (surgical/non-surgical)
- Separated instruments cannot be bypassed or removed
- Post/crown restoration requires retreatment
- Apical surgery would remove enough bone to cause a periodontal pocket
- Apical surgery would result in nerve injury or perforation of the maxillary sinus
Secondary Indications:
- To gain access to perforations on the mesial/distal or lingual root surface (esp inraradicularly)
- To treat grossly overfilled conventional root fillings and teeth with blunderbuss apices
- To enable inspection of a root for fracture
- When the patient will not accept apical surgery
- When the wrong tooth is extracted or accidental avulsion of a tooth during the removal of crown in a prosthetic procedure;
- Cases involving a deciduous tooth to allow it to act as a space maintainer
Contraindications for IR are:
- Presence of periodontal disease in which there is marked tooth mobility, furcation involvement or gingival inflammation
- Flared or curved roots
- Fractured Roots
- Patients are taking bisphosphonates
Advantages:
- Less invasive than apical surgery
- Simpler, and less equipment required c.f. apical surgery
- Improved access for inspection and resection/retropreparation
- Less soft tissue scarring
Disadvantages:
- Potential for root resorption
- Reduced access to apical pathology