Back when I was working as an Endodontist with the Australian Navy, I often mentored newly graduated dentists. There was an interesting interaction between us that would often occur. The junior dentist would come into my surgery with a question about diagnosis. They would explain a set of symptoms and then show me a radiograph. I would then ask what the pulp test result was. The new grad would then slowly back out of the room in order to return to the patient and conduct the test.
I’m not sure why the pulp testing was left off the list, but I hope I hope that by the time the junior dentist had finished their posting and moved on to a new posting that pulp testing is one of the most important tools allowing us to to diagnose. Unfortunately, there is nothing certain when it comes to pulpal diagnosis, especially when we get to the grey area of reversible/irreversible pulpitis. If we really want to know what’s happening in the pulp and periapical area of a tooth, we need to extract it, section it, and look at it under a microscope. But that’s not practical…….
Pulp testing is not 100% accurate. If it was, then diagnosis would be much easier, but it often gives us essential information that will confirm a clinical diagnosis. When it comes to vital pulps, electric and cold testing gives a positive result 81-86% of the time (Petersson & Kiani-Anaraki, 1999). In a partially or completely necrotic tooth, these modalities will give a negative result on almost all occasions. This is useful infromation to have at hand.
Here is an example from when I was doing my post-graduate training:
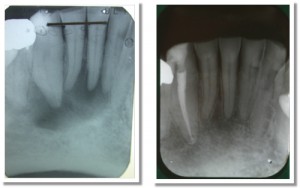
Compare these radiographs. The image on the left is the pre-op and the image on the right is the two year review.
In the case above, we can see there is a definite lucency surrounding the lower right canine and central incisor. The lateral incisor may also be involved. Pulp testing with both cold and EPT revealed the canine was testing negative and the incisors were testing positive. As only the canine was testing negative, I only treated the canine. At the two year review, we can see that the lesion has healed and normal periradicular architecture has been re-formed around the vital incisors. If we just worked from the x-rays, we’d probably treat all three teeth, and subject the patient to unnecessary treatment. This is a pretty simple lesson.
Here are the keys to successful pulp testing:
1. Make sure the teeth are completely dry and isolated with cotton wool rolls;
2. Place the tip of the pulp tester on tooth structure, not restoration, and use a small (perhaps half of a) cotton pellet or endo sponge;
3. Start your test with a tooth that you expect will give a normal result and is not involved with the area in question. This will allow the patient to get a feel for what a normal response is;
4. Test with both cold and EPT. If the patient is experiencing symptoms such as a hyper-response to hot foods/liquids, then use hot as well.
In my surgery I have the pulp tester sitting right next to me, along with things like the apex locator and endo motor. We use it that often.
References:
Petersson KS, C. Kiani-Anaraki, M. Evaluation of the ability of thermal and electrical tests to register pulp vitality Endod Dent Traumatol 1999;15:127-131.


Hi Pat,
First of all, excellent, excellent endo blog!
One of the bad habits that I picked up once I had left dental school was to make a diagnosis based primarily on radiographic signs and the patient’s reported symptoms. Soon enough, though, I ran into several puzzling cases. Pulp testing is vitally important! (No pun intended :P)
Thx for the interesting read.
Always trying to improve my diagnostic capabilities, and this was an article that will help for sure.
Any suggestions on what type of EPT unit to use???
Hi Guys,
Thanks for the comments. I happen to use the Sybron Endo Analytics electric pulp tester. Mainly because it combines apex locator and pulp tester into one unit, reducing the number of machines we need to have. Also, it comes with some nice tips for getting under crown margins.
Pat
How do you efficiently pulp test a tooth that has a full coverage restoration?
HI Joe,
You can often get a result using dry ice or even cold spray methods through a crown. Just because there is a crown, doesn’t mean you shouldn’t try with cold. The other method is to use an electric pulp tester which has a narrow probe attached to it and reflect the gingiva with a plastic instruments to allow access to the root surface. Failing these, then on occasion, you may need to prepare a test cavity through the crown.
Pat
Hi Pat,
Thanks for the insight!
May I just ask for your opinion on what the diagnosis would likely to be if EPT is positive but cold test turned out to be negative?
HI Jnn,
This situation occurs frequently when there is calcification in the coronal part of the tooth. If there is a lot of dentine insulating the pulp, then the tooth may not respond to cold, but an electric pulp tester will give you a response. An alternative situation where this might occur is where there has been partial necrosis of the pulp, so the pulp chamber contains necrotic tissue, but there is still some living tissue in the canals. The vital tissue in the canals may give a response to the EPT.
Pat
Does clod test negative mean a tooth should be extracted ?
No not necessarily Howard.
Hi Pat,
Similar to Jnn’s question, how would you interpret/treat a situation where the patient experienced a sensation during the cold but not the electric test?
Thanks for the help!
Hi Michael,
The thing with pulp testing is that the clinical situation is just as important to the test results as the test result itself. Every test has a false positive and false negative rate, so if you have a tooth that is clinically healthy otherwise (no pain, xray normal, no deep fillings) and it responds consistently to cold, then there’s a high chance the EPT test is a false negative. Conversely, if the tooth had a large carious lesion and a periapical lucency on the PA, then the cold test may be questionable. But, in this case, you wouldn’t bother doing a test as the test won’t change your management. Most situations will fall somewhere in between these, but the most important thing is to realise these tests are not 100% accurate, and consider the clinical situation and how it fits the test result.
Cheers,
Pat
Hi
What would I consider with an EPT reading of 70/80….normal or irreversible pulpits?
Hi,
The diagnosis depends much more on the symptoms than the EPT. A reading of 70/80 could be completely normal or it could happen with pulpitis. The test alone can’t make a diagnosis for you.
Pat